An Understanding of Protease Mechanisms Lead to New Treatments of HIV Infection
“…I would raise awareness to
certain causes like HIV awareness that is timely and relevant to my country,
which is the Philippines…” This is one part of Pia Wurztbach’s response to the
final Q&A of Miss Universe 2015 where she hooked the crown.
What is the real status of HIV in
the Philippines?
The case of HIV in the
Philippines increased up to 207% from 2010 to 2019 with a death toll increase
of 338%. This is considered the fastest rising in the Asia and Pacific region.
In 2019, there are about 97,000 persons living with HIV or PLHIV. The majority
of these PLHIV are persons who injected drugs, men who have sex with men, sex
workers, and transgender (Nguyen).
The virus can be transmitted
through body fluids like blood, breastmilk, semen, and vaginal secretions but
does not pass by kissing, hugging, sharing food, or drinks (“HIV/AIDS”).
Human immunodeficiency virus or
HIV is the main causative agent of acquired immune deficiency syndrome or AIDS,
which emerges in the 80s and is considered an epidemic worldwide.
HIV is a retrovirus having its
genetic information is in the form of RNA and has a reverse transcriptase
enabling the virus to use the RNA in the synthesis of complementary DNA
(Nelson, 587).
How do HIV infection proceeds?
The infection occurs when the
viral and cellular membrane fused with the facilitation of viral envelope
glycoprotein and the receptors CD4 of the target cells.
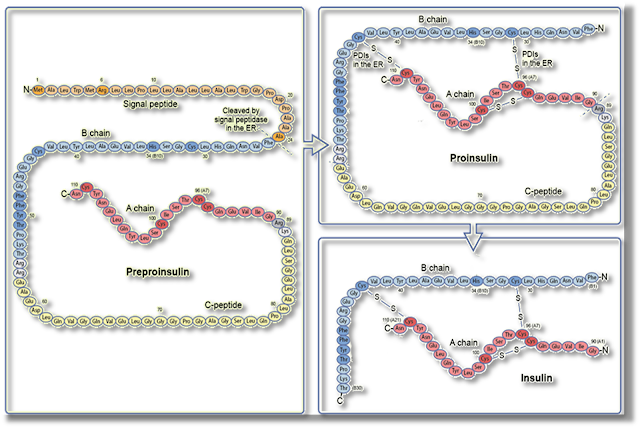
When the virus enters the cell,
its RNA is reversed-transcribed to DNA by the reverse transcriptase. The HIV
genetic material will combine with the host’s cell using the integrase enzyme
followed by transcription into the messenger RNA and replicated into viral
polyproteins. The HIV protease will incise these polyproteins to form new
virions and become ready to infect another host’s cell. With the destruction of
the host’s genetic materials and continuous production of virions results in
the death of infected cells (Brik and Wong 5–14).
 |
| Figure 1. The life cycle of HIV (“Life Cycle | NIH”) |
Based on the mechanism, there are
3 major enzymes of the HIV used in the cycle – reverse transcriptase,
integrase, and HIV protease. With these three enzymes, the HIV protease is the
most studied in the development of treatments against HIV.
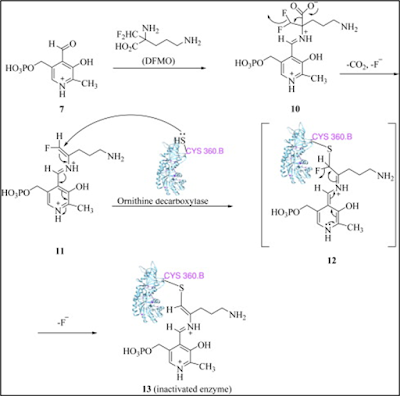
Proteases are classified into two
huge groups according to their ability to catalyze the mechanism. The first
class uses a nucleophilic atom, either hydroxyl or thiol of the amino acid side
chain to start the amide hydrolysis (Brik and Wong 5–14).
The second classification
requires two aspartyl β-carboxyl groups in the enzymatic sites to activate a
water molecule for nucleophilic reaction on a peptide bond. It is referred to
as aspartyl protease where HIV protease belongs (Windsor et al. 1465).
One way to inhibit the
proliferation of HIV is by disturbance of the HIV protease enzyme responsible
for the breakdown of polyprotein virus using protease inhibitors called
anti-retroviral or ARVs. Here are several USFDA-approved ARVs given to PLHIV
(Brik and Wong 5–14).
 |
| Figure 2. Structures of different HIV protease inhibitors or antiretrovirals. |
The different HIV protease
inhibitors vary in their structures but have similarities in terms of the main
chain with a hydroxyl group in the β-position from the benzyl group (Nelson,
589).
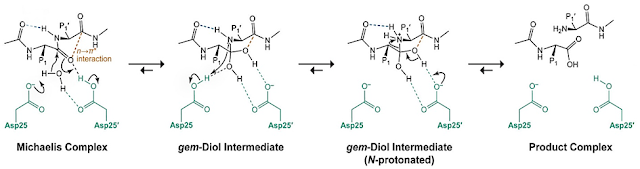
Refer to the figure below
regarding one of the accepted mechanisms for the aspartyl protease (HIV
protease) mechanism.
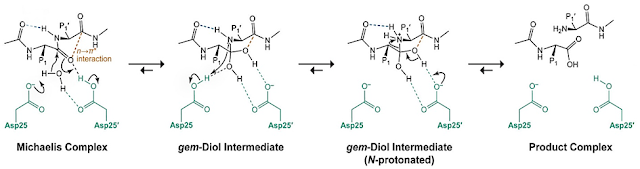 |
| Figure 3. One of the acceptable mechanisms of HIV protease. |
Studying the mechanisms for HIV
protease enzyme, and other enzymes is a good starting point in the discovery of
new drugs that can cure (or at least control its progress) not only HIV but
also other chronic illnesses. The available ARVs help extend the lifespan of
the PLHIV.
Recently, there is a reported
case of PLHIV cured of the said retrovirus. The patient undergoes stem cell
treatment using cord blood with the mutation that prevents the entrance of HIV
into the cell. Thirty-seven (37) months after the transplant, the patient
chooses to top the use of ARVs. After 14 months, the patient did not show any
signs of HIV in the blood tests as well as detectable antibodies to the virus
(Mandavilli).
With this information, it can be
a great breakthrough for researchers to further study the mechanism on how the
stem cell procedure works in killing the HIV in the body which will lead to the
right medicine or drug in the cure of this incurable disease.
References:
Brik, Ashraf, and Chi-Huey Wong. “HIV-1 Protease:
Mechanism and Drug Discovery.” Organic
& Biomolecular Chemistry, vol. 1, no. 1, 2002, pp. 5–14. Crossref, https://doi.org/10.1039/b208248a.
“HIV/AIDS.” WHO, 30 Nov. 2021, www.who.int/news-room/fact-sheets/detail/hiv-aids.
“Life Cycle | NIH.” CLINICAL INFO.HIV.GOV,
clinicalinfo.hiv.gov/en/glossary/life-cycle. Accessed 21 Mar. 2022.
Mandavilli, Apoorva. “A Woman Is Cured of
H.I.V. Using a Novel Treatment.” The
New York Times, 22 Feb. 2022, www.nytimes.com/2022/02/15/health/hiv-cure-cord-blood.html.
Nelson, David. Lehninger Principles of Biochemistry.
7th ed., W.H. Freeman, 2017.
Nguyen, Alice. “The HIV Epidemic in the
Philippines: Affected Populations.” The
Borgen Project, 26 Jan. 2021,
borgenproject.org/hiv-epidemic-in-the-philippines.
Windsor, Ian W., et al. “An N→π* Interaction
in the Bound Substrate of Aspartic Proteases Replicates the Oxyanion
Hole.” ACS Catalysis,
vol. 9, no. 2, 2018, pp. 1464–71. Crossref,
https://doi.org/10.1021/acscatal.8b04142.